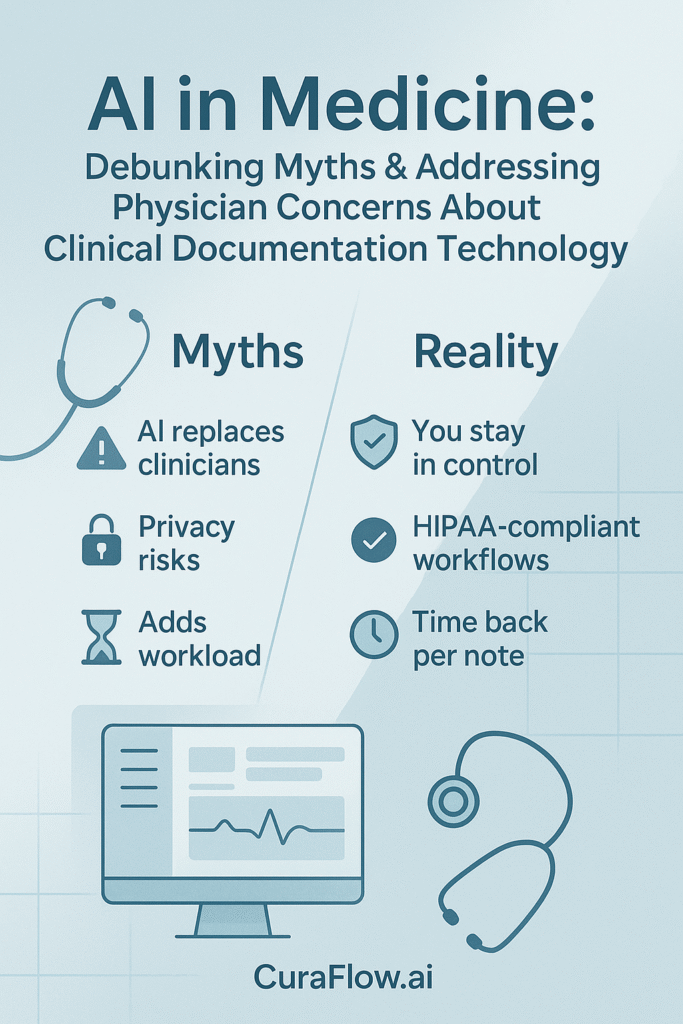
Summary: AI is already reshaping healthcare, but documentation tools raise valid questions about trust, privacy, and workflow fit. This article separates myths from realities and outlines practical safeguards so clinicians can evaluate AI on its merits.
Myth 1: “AI will replace doctors.” Think augmentation, not substitution
Today’s clinical AI excels at pattern recognition and automating repetitive tasks. It does not replace clinical reasoning, ethics, or empathy. In documentation, AI acts as an assistant: capturing encounters, organizing information, and suggesting codes so physicians can focus on decisions and patient care.
CuraFlow.ai follows a “Human Expertise + AI Power” model that enhances, not supplants, the clinician’s role.
Myth 2: “AI is a black box I can’t trust it.” Keep control with transparent workflows
Documentation tools aren’t making independent medical judgments. They learn structure and language to draft notes based on what you say and do. The physician reviews, edits, and signs the record. Look for:
-
Full editability and attribution
-
Clear audit trails
-
Transparent data handling and permissions
-
Bottom line: AI can streamline the first draft while clinical judgment stays with you.
Myth 3: “AI is only for large hospitals with big budgets.” Small practices can benefit most
Modern tools are accessible and scalable for solo and small practices. Time saved per note can mean a few more patients, fewer after-hours charts, or simply evenings back. The key is right-sized onboarding and early QA so value appears in week one.
CuraFlow.ai focuses on practical implementation for smaller teams, minimizing disruption and accelerating time-to-value.
Concern 1: “Is my patient data secure?”
Security is non-negotiable. Reputable vendors align with privacy regulations (e.g., HIPAA in the U.S.) and back their responsibilities with a Business Associate Agreement (BAA) when PHI is involved. Require the following from any documentation partner:
-
Encryption in transit (TLS) and at rest
-
Role-based access control with least-privilege permissions
-
Audit logs for access and edits
-
Data retention & deletion policies you can review
-
Breach notification procedures and defined SLAs
-
BAA and clear statements on subcontractors and data locations
CuraFlow.ai recommends only HIPAA-appropriate workflows and requires BAAs for PHI. Our onboarding process includes a comprehensive privacy checklist (covering data flows, access roles, and retention) to ensure clinicians are aware of exactly where data resides and who has access to it.
Concern 2: “Will AI create more work or disrupt my clinic?”
Poorly implemented tools can add friction. Well-designed systems do the opposite:
What “seamless” looks like
-
Quick capture (ambient or active dictation) → clean first draft in your note
-
Specialty-tuned templates that reflect your documentation patterns
-
Minimal clicks to review, edit, and sign
-
Early QA + peer tips during weeks 1–4 to lock in efficient habits
How CuraFlow.ai implements
-
Practice assessment → right-sized tool selection → guided EHR integration
-
Peer-to-peer training and live support to minimize downtime
-
Focus on measurable outcomes (e.g., time-to-first-signed note, week-4 active use)
Conclusion
Adopting AI for documentation isn’t about replacing clinicians; it’s about reducing burden while keeping clinical judgment and data control with the physician. With the proper guardrails, you gain stronger privacy, smoother workflows, and more time for patient care.
If you’re evaluating options, get our 1-page Buyer’s Checklist (transparency, editability, QA, HIPAA/BAA, audit logs, retention), mail us at support@curaflow.ai, or visit CuraFlow.ai for a vendor-neutral readiness review and week-1 adoption plan.